Introduction
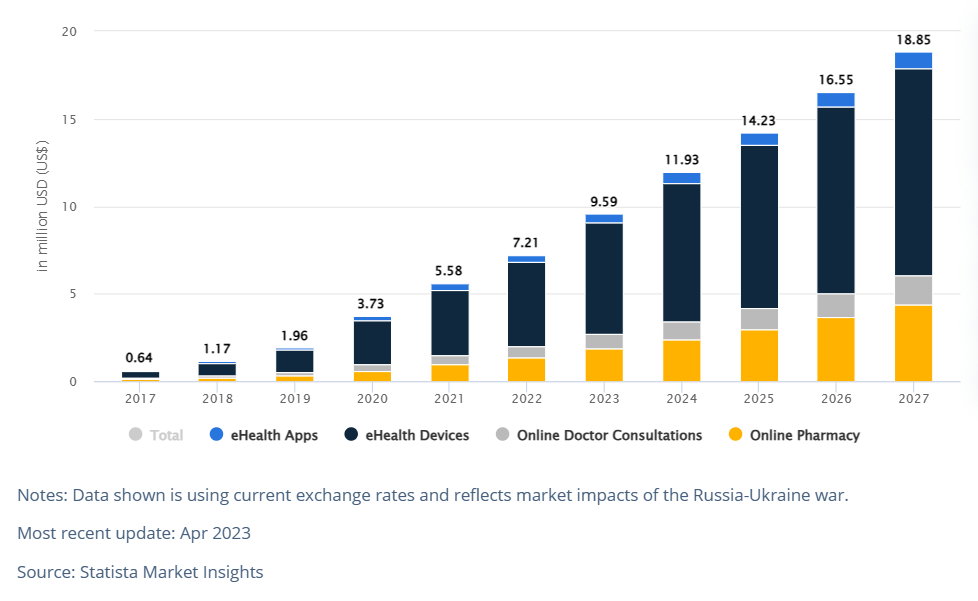
Digital health is rapidly transforming the healthcare industry, with the use of technologies such as telemedicine, telehealth, and artificial intelligence (AI) playing a significant role [1]. Smart technologies are also being adopted to improve patient outcomes and experiences [2]. Deloitte predicts that the future of health will involve a shift towards a more personalized and proactive approach, enabled by digital technologies [3]. Climate change is a global challenge that requires urgent action across all sectors, including healthcare, which is a significant contributor to greenhouse gas emissions. Many of the health risks posed by climate change require long-term planning and investment [4]. In today’s health care context, the application of the Internet of Things (IoT) offers suitability for doctors and patients as we can use them in many medical fields [5]. The healthcare industry’s carbon footprint stems from energy consumption, waste generation, and transportation, and its impact is expected to increase due to the growing demand for healthcare services worldwide. However, emerging technologies such as eHealth, “Medical Internet of Things” (MIoT) (a derivative of IoT or Internet of Things), and robotics offer promising solutions to reduce the environmental impact of healthcare. As Istepanian et al., stressed it, the use of wearables and other connected devices in health care is expected to become more common, with the potential to improve both patient outcomes and the efficiency of health care systems [6].
For instance, eHealth technologies have been widely adopted in the United States and other developed countries, enabling electronic health record systems and telehealth programs that reduce the need for paper-based records and transportation, respectively [7]. In Africa, where healthcare facilities face significant challenges due to a lack of infrastructure, resources, and healthcare services, eHealth technologies such as the National Health Information System in many African countries has the potential to enabled real-time disease outbreak monitoring, improved patient care, and reduced the need for paper-based records [8,9]. However as [10] mentioned it a decentralised approach to the implementation of HIS is more appropriate for Africa’s health systems
Furthermore, robotics technologies have the potential to transform surgical care in Africa, reducing the need for repeat surgeries and hospital visits while improving patient outcomes. For example, the Chris Hani Baragwanath Hospital in South Africa has implemented robotic surgery for prostate cancer treatment [11, 12]. One example of digital innovation in healthcare is the deployment of an innovative data system at the University of California, San Francisco, which integrates research and care to improve patient outcomes [13]. Another example is Eko Health, a digital health company that uses AI and machine learning to analyze heart sounds and identify potential heart conditions [14].
While the potential of these technologies to reduce the healthcare industry’s carbon footprint is clear, their adoption and implementation remain uneven across the globe. More research and investment are required to encourage widespread adoption of these technologies and address implementation challenges in resource-limited settings. This article will examine the advantages and disadvantages of eHealth, MIoT, and robotics in reducing the healthcare sector’s carbon footprint, as well as provide recommendations for policymakers, healthcare providers, and technology developers on how to promote sustainable healthcare practices.
I. Overview of the impact of healthcare on the climate
The healthcare industry is responsible for a significant amount of greenhouse gas emissions, with an estimated 5% of global emissions coming from the healthcare sector. The industry generates carbon footprint through energy consumption, waste generation and transportation. Healthcare facilities consume large amounts of energy to power medical equipment, heating, ventilation, and air conditioning systems. The use of single-use medical devices and packaging materials also generates a significant amount of waste. Additionally, transportation of patients, medical personnel, and supplies also contributes to carbon footprint.
II. Introduction to eHealth, MIoT, and robotics
EHealth, IoT, and robotics are examples of digital technologies with the potential to transform the healthcare industry. EHealth is the use of digital technologies to provide healthcare services, such as telemedicine, Electronic Health Recorders(EHRs), and digital medical devices. Recently, a growing trend in the healthcare industry is the emergence of a subcategory of the IoT known as the “Medical Internet of Things” (MIoT). Unlike traditional IoT devices, MIoT devices are specifically designed for medical purposes and are connected to the internet or other networks to enable communication with each other. MIoT devices allow for the sharing of important patient information in real-time, enhancing the accuracy and speed of diagnosis and treatment. This advancement has the potential to revolutionize the way medical professionals approach patient care and lead to more efficient and effective healthcare services.
MIoT entails the collection and transmission of healthcare data via interconnected devices and sensors. In contrast, robotics is the use of machines to automate processes, perform surgeries, and deliver medical supplies.
III. How eHealth can minimize the impact on the climate?
3.1. Telemedicine
Telemedicine is the use of digital technologies to deliver healthcare remotely. This reduces the need for patients and healthcare providers to travel, thereby lowering the carbon footprint. Patients can get healthcare from the comfort of their own homes, reducing the need for transportation. Remote consultations can also be provided by healthcare providers, reducing the need for patients to travel to healthcare facilities. More and more people in the healthcare industry are working with developers around the world to provide telemedicine software and platforms.
3.2. Electronic Health Records (EHRs)
The EHRs can significantly reduce paper usage and storage, which contributes significantly to the carbon footprint in healthcare facilities. EHRs allow healthcare providers to electronically access patient data, eliminating the need for paper-based records. Furthermore, electronic prescribing can reduce the need for paper-based prescriptions, reducing paper usage even further.
3.3. Digital Medical Devices
The EHRs can significantly reduce paper usage and storage, which contributes significantly to the carbon footprint in healthcare facilities. EHRs allow healthcare providers to electronically access patient data, eliminating the need for paper-based records. Furthermore, electronic prescribing can reduce the need for paper-based prescriptions, reducing paper usage even furth Wearable health monitors and mobile health apps, for example, can enable patients to manage their health remotely, reducing the need for frequent hospital visits. These devices can also monitor vital signs and notify healthcare providers of any irregularities, allowing for early intervention and reducing the need for emergency hospital visits.
Other than those, there are numerous eHealth device solutions that can help to minimize the impact on the climate. For instance, smart water bottles can track water intake and hydration levels, while smart thermostats allow for remote control of heating systems. One example of a wireless vital signs monitor is the Caretaker, which connects to an Android device and provides real-time vital sign data, including continuous beat-by-beat blood pressure, without the need for wires or invasive methods. In addition to measuring blood oxygen levels, respiration rate, core body temperature, early warning score, and blood volume levels, the device can be worn by the patient as a finger cuff and wristband. The Eko Core digital stethoscope, on the other hand, has both analog and amplified modes and can be used with a smartphone app to visualize and record sounds picked up. The device is HIPAA-approved, allowing for easy sharing of results with colleagues or patients or direct upload to electronic medical records [14]. Finally, smart injection devices are connected drug delivery devices that allow doctors and patients to monitor injection administration, support any syringe design, and share data with the doctor about the amount being administered and any common patient errors. These eHealth solutions can significantly reduce the environmental impact of healthcare while improving patient outcomes.
IV. How MIoT can minimize the impact on the climate?
4.1. Remote patient monitoring
Remote patient monitoring is the use of interconnected devices to remotely monitor a patient’s health. This reduces the need for frequent hospital visits, as well as the carbon footprint associated with transportation. Patients can also benefit from early interventions, which reduces the need for emergency room visits.
4.2. Smart healthcare facilities
Smart healthcare facilities optimize energy usage with interconnected devices and sensors, lowering energy consumption and carbon footprint. These devices can monitor energy consumption and adjust lighting, heating, ventilation, and air conditioning systems automatically to reduce energy waste. For example the smart hospital room project where IBM Watson has collaborated with Thomas Jefferson University in Philadelphia to develop a smart hospital room that is being implemented in the three hospitals overseen by the university. This partnership aims to provide a fully integrated and intelligent hospital room that can enhance patient outcomes by providing personalized care and support to medical staff.
4.3. Real-time inventory management
MIoT can also enable real-time inventory management, reducing waste from expired or unused medical supplies. Interconnected devices can monitor inventory levels and alert healthcare providers of any low supplies, reducing overstocking and waste.
V. How robotics can minimize the impact on the climate?
5.1. Automated processes
Robots can automate processes such as sterilization, cleaning, and laundry, reducing energy consumption and carbon footprint. Automated processes can also reduce the need for human labor, reducing carbon footprint from transportation.
5.2. Robotics-assisted surgery
Robotic-assisted surgery can reduce the amount of time patients spend in the hospital, reducing energy consumption and carbon footprint. Robotic-assisted surgery also has a higher success rate, reducing the need for repeat surgeries and hospital visits. IDC [15] has forecast that by 2026 two-thirds of medical imaging processes will use AI to detect diseases and guide treatment. A growing number of healthcare leaders believe that investing in AI technology is important for the future of their medical facility, according to the Royal Philips report.
5.3. Autonomous delivery of medical supplies
Robots can also be used to deliver medical supplies autonomously, reducing carbon footprint from transportation. Autonomous delivery can also reduce the risk of human error, ensuring that medical supplies are delivered on time and in the correct quantity. Swisslog and Savioke have introduced a new autonomous service robot to the healthcare industry, which can perform tasks such as delivering medication and supplies to patients [16].The robots are equipped with sensors to navigate through hospital hallways and elevators, and can even open doors using RFID technology. This not only reduces the carbon footprint from transportation but also reduces the risk of human error and frees up hospital staff to focus on patient care.
VI. Challenges of implementing eHealth, MIoT, and robotics
6.1. Cost
The implementation of eHealth, MIoT, and robotics can be costly, making it difficult for some healthcare providers to adopt these technologies.
An example of the cost of implementing these technologies can be seen in the case of the University of California San Francisco Medical Center (UCSF), which implemented an electronic medical records system [13]. The system cost you could tell is over $100 million to implement and resulted in significant operational and financial challenges for the organization. Other healthcare providers have faced similar challenges with the cost of implementing new technologies, which can include hardware, software, training, and ongoing maintenance costs. These costs can be prohibitive for smaller healthcare providers with limited budgets, making it challenging for them to keep up with the latest technological advancements.
6.1. Privacy and security concerns
The use of digital technologies in healthcare raises privacy and security concerns. Healthcare providers need to ensure that patient data is protected and secure. With the increasing reliance on technology in healthcare comes the risk of cybersecurity breaches. For instance, the Anthem healthcare breach in 2015 was the largest healthcare breach in history, affecting 78.8 million individuals [17]
In 2015 Hackers were able to steal from Anthem, Inc personal information, including names, birth dates, social security numbers, and healthcare ID numbers, from approximately 80 million Anthem customers. This breach was a wake-up call for the healthcare industry, highlighting the need for stronger security measures to protect patient data. As the use of digital technologies in healthcare continues to grow, it is crucial for healthcare providers to implement robust security protocols to safeguard patient data.
6.1. Resistance to change
Resistance to change can also be a barrier to the adoption of eHealth, MIoT, and robotics. Healthcare providers may be reluctant to adopt new technologies, preferring traditional methods. A tangible example of resistance to change in healthcare technology can be seen in the slow adoption of electronic health records (EHRs) by some healthcare providers. Despite the many benefits of EHRs, such as improved patient safety, reduced medical errors, and increased efficiency, some providers still prefer to use paper records. This resistance to change can be due to various reasons such as cost, lack of training, and fear of technology failure.
VII. Recommendations and conclusion
The adoption of eHealth, MIoT, and robotics technologies has the potential to reduce the healthcare sector’s carbon footprint significantly. However, the adoption and implementation of these technologies remain uneven across the globe, and several challenges and limitations must be addressed to promote sustainable healthcare practices.
Policymakers can encourage the use of eHealth, MIoT, and robotics by providing incentives such as tax credits and subsidies. Healthcare providers can also be encouraged to adopt these technologies by providing training and support.
Investing in research and development can help overcome the challenges of implementing eHealth, MIoT, and robotics. Research can also help identify the most effective and efficient ways to implement these technologies.
Regulations and standards as to be established to help ensure that eHealth, MIoT, and robotics are used ethically and responsibly. Regulations can also help protect patient data and ensure that healthcare providers adopt these technologies safely.
In conclusion, the issue of climate change continues to be a major concern for the future of our planet. With increasing levels of carbon emissions and rising global temperatures, the effects on our environment are becoming more evident each year. From devastating natural disasters to the extinction of species, the impact of climate change is far-reaching and complex. However, with increased awareness and global cooperation, we can work towards mitigating the effects of climate change and finding sustainable solutions for the future. By reducing our carbon footprint, investing in renewable energy, and promoting environmentally friendly practices, we can help to ensure a brighter and more sustainable future for ourselves and future generations. Adoption of eHealth, MIoT,and AI powered technologies has the potential to reduce the carbon footprint, optimize energy consumption, and improve patient outcomes. However, eHealth, MIoT, and robotics implementation faces challenges such as cost, privacy and security concerns, and resistance to change. To overcome these obstacles, policymakers, healthcare providers, and technology developers must collaborate to promote the use of these technologies. This can be accomplished by providing incentives, investing in R&D, and establishing regulations and standards. By doing so, we can build a more resilient and sustainable healthcare system that is better prepared to face the challenges of climate change.
References
[1] World Economic Forum. (2021, May 14). How digital health is set to revolutionize the healthcare industry. https://www.weforum.org/agenda/2021/05/digital-health-telemedicine-telehealth-ai-digitalize-health-services/
[2] World Economic Forum. (2021, October 5). How smart technologies are transforming healthcare.https://www.weforum.org/agenda/2021/10/smart-technologies-transforming-healthcare/
[3] Deloitte. (n.d.). Future of health. https://www2.deloitte.com/global/en/industries/life-sciences-health-care/perspectives/future-of-health.html
[4] Davis, J., & Nolan, K, Climate change and the global health emergency. Harvard Business Review, vol. 95, no. 1, pp. 121-128, Jan.-Feb. 2017.
[5] M.A. Khan, “Challenges Facing the Application of IoT in Medicine and Healthcare,” International Journal of Computations, Information and Manufacturing (IJCIM), 2021
[6] Istepanian, R., Hu, S., & Philip, N. (2018). Wearables and the Internet of Things for Health: Wearable, Interconnected Devices Promise More Efficient and Comprehensive Health Care. Journal of Medical Internet Research, 20(5), e162.
[7] Journal of Healthcare Engineering, vol. 2018, Hindawi, 2018.
[8] African Journal of Primary Health Care & Family Medicine. (2018). [Online]
[9] Lucia M. Mupara, John J.O. Mogaka, William R. Brieger, Joyce M. Tsoka-Gwegweni,Community Health Worker programmes’ integration into national health systems: Scoping review, African Journal of Primary Health Care & Family Medicine | Vol 15, No 1 | a3204 | DOI: https://doi.org/10.4102/phcfm.v15i1.3204 | © 2023 Lucia M. Mupara, John J.O. Mogaka, William R. Brieger, Joyce M. Tsoka-Gwegweni | This work is licensed under CC Attribution 4.0 Submitted: 18 August 2021 | Published: 09 March 2023
[10] Oluwamayowa O. Ogundaini, Mourine S. Achieng,Systematic review: Decentralised health information systems implementation in sub-Saharan Africa,The Journal for Transdisciplinary Research in Southern Africa|Vol 18, No 1 |a1216|DOI: https://doi.org/10.4102/td.v18i1.1216 | © 2022 Oluwamayowa O. Ogundaini, Mourine S. Achieng This work is licensed under CC Attribution 4.0 Submitted: 25 March 2022 | Published: 30 August 2022
[11] Van der Poel H, Van Cleynenbreugel B, Ngugi P, Connolly SS, Catto JWF. Robotic prostatectomy in Africa: a preliminary report from the largest robotic prostatectomy centre in Africa. World J Urol. 2019;37(1):65-72. doi: 10.1007/s00345-018-2387-2.
[12] Okhunov, Z., Rais-Bahrami, S., George, A. K., Waingankar, N., & Duty, B. D. (2019). The impact of robotic-assisted surgery on hospital system costs: systematic review and meta-analysis. World Journal of Urology, 37(7), 1381-1388.
[13] University of California San Francisco. (2022, April 4). UCSF deploys innovative data system to integrate research and care. https://www.ucsf.edu/news/2022/04/422566/ucsf-deploys-innovative-data-system-integrate-research-and-care
[14] Eko Health. (n.d.). AI-powered digital stethoscope. https://www.ekohealth.com/
[15] Mutaz Shegewi , Adriana Allocato , Giulia Besana, Cynthia Burghard, Lynne Dunbrack , Nino Giguashvili , Ramon T. Llamas , Silvia Piai , Jeff Rivkin , Michael Townsend , Manoj Vallikkat , Leon Xiao, IDC FutureScape: Worldwide Health Industry 2021 Predictions, https://www.idc.com/research/viewtoc.jsp?containerId=US45834920
[16] Robotics and Automation News. (2018, October 23). Swisslog and Savioke introduce new autonomous service robot to healthcare industry. https://roboticsandautomationnews.com/2018/10/23/swisslog-and-savioke-introduce-new-autonomous-service-robot-to-healthcare-industry/
[17] Infosec Institute. (n.d.). The breach of Anthem Health: The largest healthcare breach in history. https://resources.infosecinstitute.com/topic/the-breach-of-anthem-health-the-largest-healthcare-breach-in-history/